5 EHR Optimization Strategies for Maximizing Efficiency and Productivity
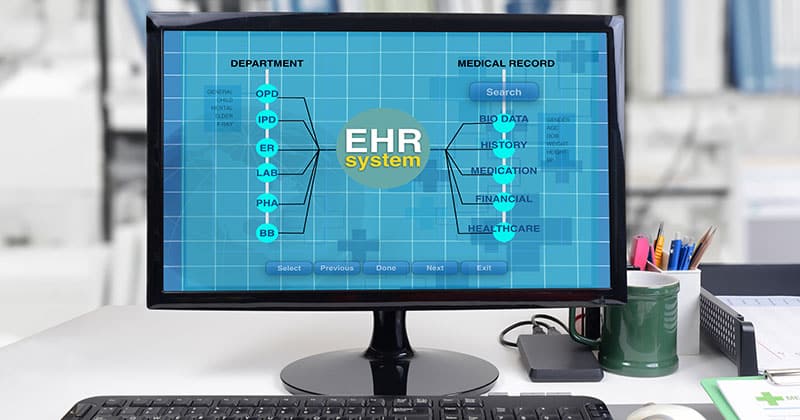
In healthcare, every second counts. Electronic health record (EHR) systems are at the h...
February 20, 2024
Electronic health records (EHRs) have simplified tasks for patients and medical providers, yet despite the added convenience, they have also raised concerns about EHR security.
Employing high-level EHR security measures improves patient experience and retention. It also keeps your organization compliant with laws pertaining to patient medical records.
Learn how to safeguard patient data with these expert tips.
Electronic health records have become the standard for collecting and sharing patient data, but online storage also opens the door to privacy violations and theft.
Patient files are breached or stolen for a variety of reasons, including:
Personal data at this level can be very lucrative for thieves on the black market. In some cases, entire criminal enterprises are devoted to ID theft and insurance fraud. In other instances, the perpetrators are lower-level criminals who still cause major damage to a patient’s credit and identity.
FROM ONE OF OUR PARTNERS: 5 Healthcare Data Security Threats to Watch For
Naturally, breaches in healthcare data can have devastating effects on patients. They may find someone has stolen their identity to open credit cards in their name.
Patients’ names may be associated with purchases of controlled pharmaceutical substances or targeted by phishing phone calls that sound legitimate because scammers have obtained their personal information.
A data breach is not a trivial concern. In 2021, over 40 million patient records were compromised. The largest breach affected over 3 million people, and those were just the cases reported to the federal government. There is no doubt that some incidents go undetected and unreported.
Patients are not the only parties affected by the mishandling of data. Breaches in EHRs are equally damaging for healthcare providers.
Some possible consequences include:
Your patients and colleagues rely on the safeguarding of EHRs. Violations of their trust and privacy have far-reaching effects, which is why security regulations to govern the protection of patient information and EHRs have been implemented. The primary laws are outlined in HIPAA, the Health Insurance Portability and Accountability Act.
HIPAA not only requires EHRs to be current and accurate, but it also mandates that health data be kept secure in use and transfer.
If EHRs purport to be safe, how do criminals get their hands on patient records that should be private? Cybercriminals use a variety of methods to get around HIPAA, including:
The most vulnerable point of any secure system is human error. Many cybercriminals prey on clinic or hospital employees with convincing scams, such as phishing emails that look legitimate but are from questionable sources.
If the recipient answers, criminals get the information they want quickly, without the recipient realizing they’ve been compromised until much later. Training staff to avoid these tactics is your practice’s best defense.
Looking at the vulnerabilities above, you’ll see they have something in common: they’re largely preventable.
Here are actionable steps your medical practice can take to reduce illegal EHR access and data theft.
The first thing your practice should do to protect patient information is to choose EHR management systems with an established reputation for safety and reliability. Read reviews from other practices and research companies online to see if any confirmed breaches have been reported.
Likewise, any cloud storage systems you use must be secure. Often, cloud storage is integrated with EHR platforms, but if you also use on-site storage servers, consider taking these steps:
Your patients’ health records are only as secure as the latest software versions. Be sure to update when new versions are available.
Though it can seem annoyingly frequent, your software is often updated to elevate security, not solely for new features or conveniences. Updates help the software stay a step ahead of potential hackers or close any detected security gaps in the system. Failure to update could leave your data vulnerable to theft.
FROM ONE OF OUR PARTNERS: 4 Cybersecurity Trends in Healthcare You Should Be Aware Of
One situation where patient data is particularly vulnerable is in transit between providers and practices. If you send a patient’s EHR from your general physician practice to a surgeon’s office, it is potentially at risk.
Patient data should always be encrypted. Even if this is not a requirement by law, it is still considered the gold standard for protecting patient records and gives providers and patients added peace of mind.
What is encryption, and how does it increase security? Encryption is the digital process of coding information so it can only be accessed and viewed by authorized parties. It not only protects your patients’ information from being hacked or stolen, but it also prevents unauthorized access in case information is ever inadvertently sent to the wrong recipient.
Your medical practice should employ encryption when transferring medical records, referrals, test results, and prescriptions.
Be aware that encryption standards vary between institutions and geographic locations. You may need to use higher standards when transferring information out of state, for example. Providers should also be aware of and adhere to non-U.S. regulations when sending records globally, such as for patients traveling or living abroad.
Everyone in your practice does not necessarily need access to patient files. Limit the number of people who deal with patient EHRs. Limited access reduces the number of opportunities for both intentional and inadvertent breaches and makes existing security gaps more visible, should you have to pinpoint them.
Another way to control access is to only use specified digital devices for viewing and altering patient data. Tablets carried from room to room with providers are more secure than having a computer in each exam room.
If you must use desktop computer stations, ensure employees log off immediately after use and add an automatic log-off feature for good measure.
Limit or prohibit the use of personal devices to access medical records. In the past, physicians may have brought paper charts home to get caught up on dictation and paperwork, or they were allowed to log in to medical records from their home computers when they first became digitized. We know now that offsite access creates a security vulnerability you must avoid.
That’s not to say that situations in which practitioners need access to records while away from the practice won’t arise. If this is common or expected, provide the practitioner with a secure laptop with proper encryption functions installed strictly for work use.

You can see that patient records are only as safe as the employees working with them. Every new employee should be trained in data security, and there should be annual refresher training sessions to cover any new regulations and security protocols.
Employees should take care not to leave computer screens open after use. In busy departments—especially the emergency room—it’s all too easy to leave windows open to reduce time at the keyboard.
Staff must also be kept abreast of current phishing and other email scams used to steal sensitive patient information. If they have any doubt about the validity of an email or other correspondence, they should run it by a clinic supervisor or IT professional.
FROM ONE OF OUR PARTNERS: EHR Implementation Check-list: 5 Steps to Simplify the Process
Rather than adding medical information safety measures piecemeal, establish an official process so that providers and staff have direct instructions for handling security questions as they arise. These steps will help you create a formal process for safeguarding patient data:
If you are concerned about the security of patient electronic records in your medical practice, follow these steps today to improve data safety. Your patients will appreciate knowing their information is secure, and you can rest easier knowing your clinic goes above and beyond HIPAA compliance.
Ensure all software and storage systems you use are at least HIPAA compliant and ONC-ATCB certified. Some systems now exceed government requirements for the highest level of security. For example, systems with additional encryption measures for the transfer of patient EHRs.
Use an audit trail feature to track record access. Many current EHR programs include the ability to audit who has accessed patient records. Be sure to enable this feature so that you can see who was involved in a breach and act accordingly.
Always use strong password protections. This is common advice across all online activities, especially when dealing with sensitive information. Passwords should be a minimum of 16 characters and contain uppercase letters and special characters. They should also be reset at regular intervals. Staff password access should be removed immediately upon termination of their employment.
In a professional setting, adding a lockout feature for entering the wrong password several times can be beneficial.
You may also want to consider adding two-factor authentication as another security layer. This involves sending a verification code by email or text when someone logs in to the system.
Two-factor authentication may be complicated for providers who use different computers throughout the day, but it’s simple to add for staff tied to one computer who may only log off for breaks and at the end of the day.
Remember that your EHR information may be integrated with other digital systems. Be sure that any systems utilized in-office or externally, such as scheduling and billing, are also compliant.
FROM ONE OF OUR PARTNERS: Understanding the Importance of HIPAA Compliance in Medical Billing Software